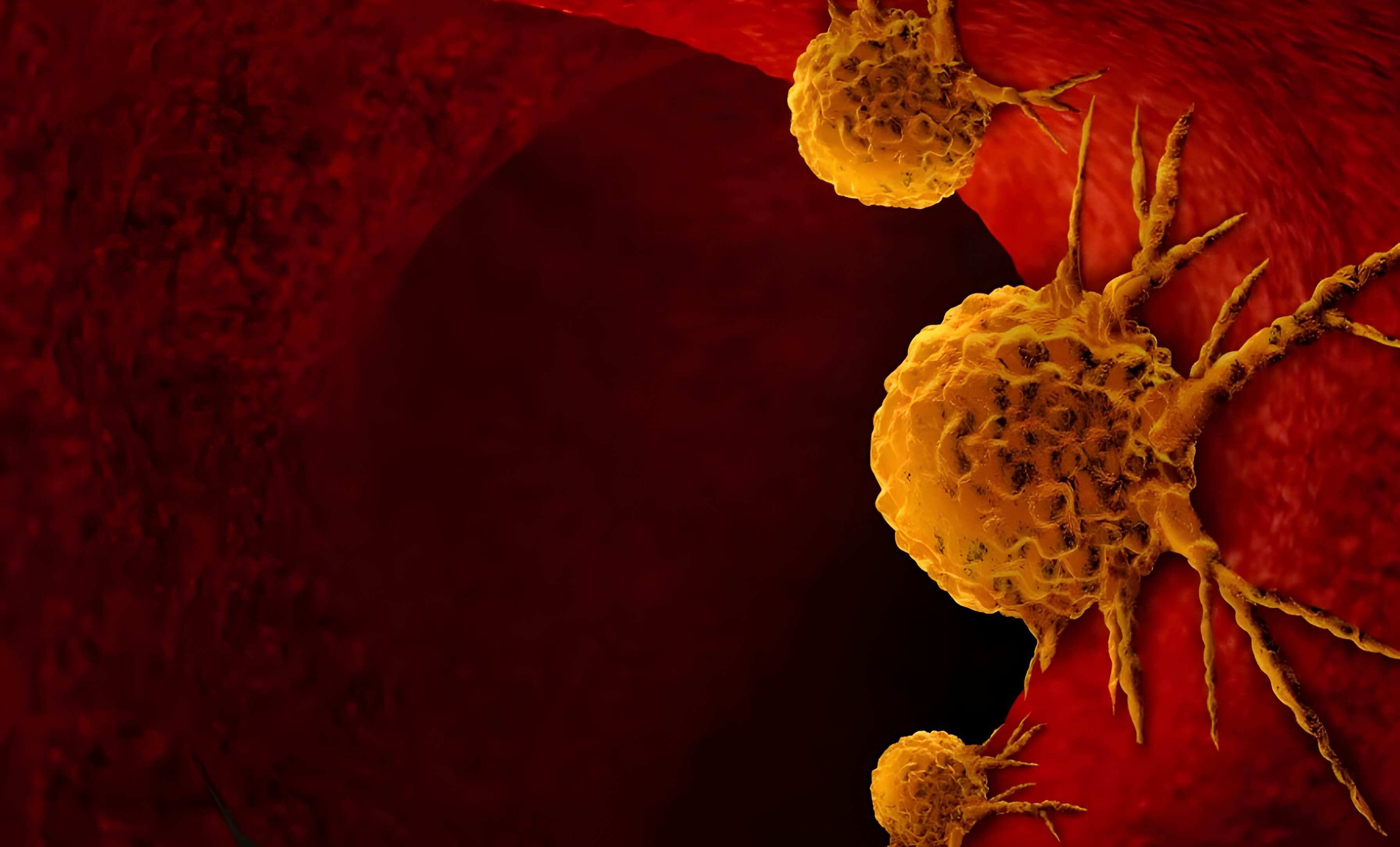
The ASEAN region’s health challenges encompass a diverse range of risks. The convergence of non-communicable diseases (NCDs), infectious diseases, climate change impacts, and other non-health factors paints a complex picture. NCDs, such as cardiovascular diseases, cancers, chronic respiratory ailments, and diabetes, are already the leading causes of death in the region, accounting for 62 per cent (8.5 million) of all fatalities.
Southeast Asia’s populations are also rapidly ageing. While this signifies progress in healthcare, people live longer but not necessarily healthier. It brings along the challenge of increased pressure on healthcare and management systems. Economic growth and rapid urban expansion may elevate the risk of NCDs through unhealthy lifestyle choices and trends. These include tobacco and alcohol consumption, lack of physical activity, and poor dietary choices.
The ASEAN region continues to be at risk of emerging and re-emerging infectious diseases. The COVID-19 pandemic showed the magnitude of the devastation that infectious diseases can wreak on the population. Experts predict similar deadly outbreaks are near the horizon due to urban growth, international travel, human-animal proximity, antimicrobial resistance, and environmental degradation. The region will also continue battling vector-borne diseases such as dengue and malaria, and respiratory illnesses.
Climate change brings in a new set of health impacts. Rising temperatures have caused and will continue to cause heat-related illnesses, worsen air quality, lead to respiratory problems, and disrupt food production, possibly leading to food insecurity and malnutrition.
The combination of health and non-health risks places Southeast Asia in a position of heightened global vulnerability, demanding a holistic and robust approach to protecting public health.
Responding to public health emergencies: Lessons from the pandemic
ASEAN has long recognised the need to strengthen the health systems of its Member States and safeguard public health. Under its ASEAN Post- 2015 Health Development Agenda, the sector tackles key priorities under four clusters: effectively responding to hazards and emerging threats, reinforcing health systems and healthcare accessibility, encouraging healthy habits, and ensuring food safety.
Existing mechanisms developed under such an agenda were mobilised by the health sector in its COVID-19 pandemic response. These include technical exchange platforms such as the ASEAN Emergency Operation Centre Network, the ASEAN Plus Three Field Epidemiology Training Network, and the ASEAN BioDiaspora Virtual Centre for big data analytics and visualisation. Resources for vaccine capacities were mobilised through the ASEAN Vaccine Security and Self-Reliance and its regional strategic framework.
In the ASCC Policy Brief No. 1 (2023) titled “Strengthening ASEAN Public Health Emergency Measures,” experts stress the importance of tailored strategic actions to address diverse health security risks within ASEAN. The pandemic has revealed weaknesses in the region’s existing health infrastructure’s ability to prevent, detect, and respond to health emergencies.
The policy brief notes that the ASEAN Member States still have much to do to achieve self-sufficiency in vaccines, therapeutics, and diagnostics and enable swift emergency responses. Limitations in resources, manufacturing, lab capacities, and health worker capabilities strain the region’s health systems. Health insurance and social protection programs alleviate the burden on vulnerable populations, while their absence can disrupt health systems. Financing is a significant challenge for universal health care and social protection.
ASEAN has strengthened regional and international partnerships to establish other mechanisms like the ASEAN Centre for Public Health Emergencies (ACPHEED), which will operate from Indonesia, Thailand and Viet Nam and coordinate multiple health-related initiatives. It is envisioned to strengthen
ASEAN’s capabilities to prepare, detect and respond to public health emergencies. As the policy brief indicates, ACPHEED is an essential step in addressing the gaps in public health emergencies.
Furthermore, the ASEAN Regional Capacity on Disaster Health Management (ARCH) project, supported by the Japan International Cooperation Agency (JICA), was first implemented from 2016 to 2021 (see page 15).
Enhancing health system resilience
While ASEAN is building its capacity to respond to public health emergencies, it is concurrently pursuing initiatives to strengthen health systems towards robust health security. Investing in resilient health systems (RHS) that can prepare for shocks, minimise the negative impacts, recover quickly, and learn lessons to be more prepared for future disruptions is essential.
ASCC’s Policy Brief No. 7 (2023), “Building Health System Resilience in ASEAN”, takes stock of the progress ASEAN has made in helping Member States improve RHS. It cites health and non-health factors contributing to RHS, including the WHO health system’s building blocks toolkit and Universal Health Coverage (UHC): service delivery, human resources for health (HRH), health and information systems, medical products and technology, financing, and leadership and governance.
The health sector has developed the ASEAN Medical Device Directive to facilitate access to diagnostic and life-saving apparatus and other medical devices.
HRH or essential workforces— doctors, nurses, medical technologists, epidemiologists, pharmacists and community health workers—are necessary for resilient health systems. ASEAN has prioritised building the capacities and capabilities of its health workforce, pushing for better compensation and recognition of their contributions.
The environment and social conditions in which health systems exist significantly influence an individual’s access to and use of health services. The brief points out that building more efficient information systems and infrastructure and promoting digital literacy can help improve the quality of medical care and access to it.
Some Member States have achieved 100 per cent universal health coverage, while others are making substantial progress towards providing affordable healthcare for their population. The experts say there is a need for Member States to invest more in public health investments and decrease the reliance on household health spending.
Another key recommendation is strengthening primary health care services to improve access to health solutions at the community level and integrating them with disaster health management initiatives.
Promoting health and preventing diseases
The COVID-19 pandemic disrupted healthcare systems, delaying screenings and treatments for many NCDs. At the same time, the stress and changes in daily routines during the lockdowns have led to unhealthy lifestyle choices and mental health issues. The WHO has sounded the alarm. In a May 2023 report, the WHO cautions that by about 2050, despite advancements in general health, the rising burden of NCDs will be responsible for 86 per cent of the global death toll of 90 million if current trends persist. The numbers represent a 90 per cent increase in absolute figures since 2019.
ASEAN Member States have made headway in promoting a healthy lifestyle, including NCD prevention programs, tobacco control, reducing harmful alcohol consumption, and prevention of injuries. ASEAN has various initiatives to promote healthy ageing, mental health, and healthy diets.
ASEAN must sustain this momentum. The ASSC’s upcoming Trend Report on Promoting a Healthy Lifestyle (2023) says that a holistic and multi-sectoral approach is required to coordinate these initiatives and empower individuals and communities to take action on their health. The report again highlights the importance of a robust healthcare system with capable professionals promoting healthy living and preventing disease.
Speaking before the WHO Executive Board in January 2022, Director-General Tedros Adhanom Ghebreyesus outlined critical priorities for the world and the WHO. The top priority was “to support countries to make an urgent paradigm shift towards promoting health and well-being and preventing disease by addressing its root causes.” He stressed that “the highest attainable standard of health does not only mean the highest attainable standard of care. It means keeping people healthy and preventing the need for care. It means true health care, not sick care.”
The public health sector needs to work in tandem with communities and individuals to combat NCDs and foster healthier lifestyles.
References may be downloaded from the following link: https:// bit.ly/Issue29_Rev
The ASEAN Issue 15-16, COVID-19 Vaccines for All: https://bit.ly/ TheASEAN_Vaccines
The ASEAN Issue 07- 08, Stronger Health System: https:// bit.ly/TheASEAN_ Stronger_Health_ System