It has been almost two years since the outbreak of the SARS-COV-2 virus, which caused the COVID-19 pandemic, and the global community is still battling against its devastating impact. So far, the disease has resulted in millions of cases and deaths worldwide, loss of livelihood, economic downturns, and disruptions in trade and the flow of essential goods and other supplies.
It is now a race against the mutation and spread of SARS-COV-2, even as COVID-19 vaccines rollout are Photo Credit: © seisler/Shutterstock ongoing worldwide. National policy and programmes on COVID-19 response are constantly being developed, implemented, revisited, and viewed by every country, including the ASEAN Member States, to respond appropriately to the pandemic and ensure a flexible but steady journey towards recovery. To complement the COVID-19 vaccine rollout campaigns and programmes, sustaining tried and tested public health and social measures for infection prevention and control are continuously advocated and enforced by the ASEAN Member States. Several vaccine-producing ASEAN Member States have also endeavoured to contribute to COVID-19 vaccine development to address the mutating SARS-COV-2.
SARS-COV-2 and Its Variants
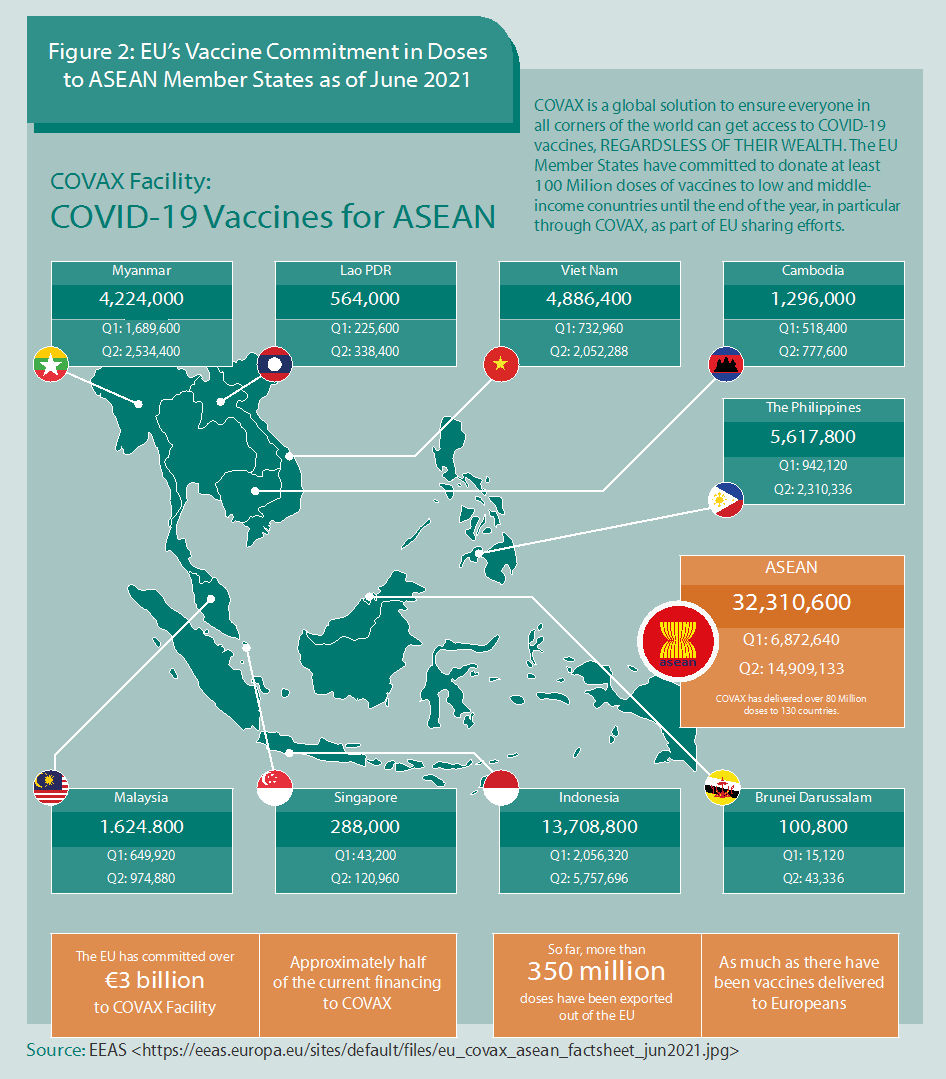
Since the December 2019 alert on cases of a respiratory syndrome of unknown cause in China, the World Health Organization (WHO) says the virus has spread to more than 220 countries and territories. Nearly 231 million cases of COVID-19 have been documented globally, with almost five million deaths as of 22 September 2021 (WHO, 2021; ASEAN, 2021). Around this period, the ASEAN region accounted for more than 11 million cases, with an upward epidemiologic trend (Figure 1) in most of the ASEAN Member States and more than 254,000 deaths. Owing to the virus’s characteristics and its widespread transmission in populations, the likelihood of viral mutations has increased. The recent surge of confirmed cases and deaths in many countries have been attributed to the variants of concern (WHO, 1 March 2021) of the SARS-COV-2 virus.
Based on the COVID-19 Weekly Epidemiologic Update published by the WHO, as of 14 September 2021, cases of the Alpha variant were reported in 193 countries, territories, and other areas. The Beta variant was detected in 142 countries; the Gamma variant in 96 countries; and the Delta Variant in 180 countries (WHO, 14 September 2021). The recent uptrend in infections, due to the increased cases of the Delta Variant, has also been reported in the ASEAN Member States. More stringent policies have been brought back to contain the spread of this more communicable variant in communities and to prevent the overwhelming of the already fragile health systems in the region.
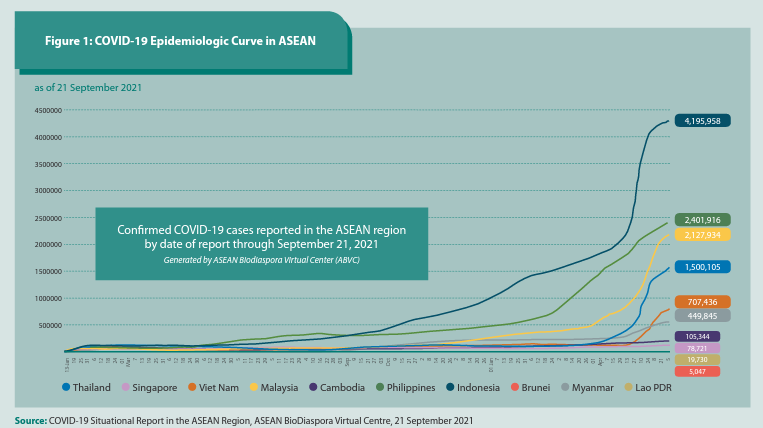
According to the WHO, the emergence of SARS-COV-2 variants, which posed an increased risk to global public health, necessitated the characterisation of variants of interest and variants of concern (WHO, n.d.). In late 2020, the WHO began classifying the SARS- COV-2 variants to reinforce global efforts on monitoring and research, and to provide information on the ongoing response to the COVID-19 pandemic. Assessing the evolution of the virus and its variants is a global undertaking, and the WHO has been monitoring it with partners, expert networks, national authorities, institutions, and researchers since January 2020.
A variant of interest (VOI) is defined by the WHO as a SARS-CoV-2 variant with genetic changes that are predicted or known to affect virus characteristics such as transmissibility, disease severity, immune escape, diagnostic or therapeutic escape. It is also identified to cause significant community transmission or multiple COVID-19 clusters in multiple countries with increasing relative prevalence alongside increasing number of cases over time, or other apparent epidemiological impacts to suggest an emerging risk to global public health (WHO, n.d.; emphasis added). The current VOIs, and where they were first identified include Eta (multiple countries), Iota (US), Kappa (India), and Lambda (Peru). (Table 1).
A variant of concern (VOC), on the other hand, is defined as a SARS-CoV-2 variant that meets the definition of a VOI and, through a comparative assessment, has been demonstrated to be associated with one or more of the following changes at a degree of global public health significance namely, increase in transmissibility or detrimental change in COVID-19 epidemiology; or increase in virulence or change in clinical disease presentation; or decrease in effectiveness of public health and social measures or available diagnostics, vaccines, therapeutics (WHO, n.d.; emphasis added). (Table 2)
Public Health and Social Measures
Public Health and Social Measures (PHSM) are comprised of interventions implemented not only by international organisations and national and local governments but also by organisations, communities, and individuals to curb the spread of COVID-19 and other communicable diseases. Wearing of appropriate masks, frequent hand washing, and observance of social distancing are just some of the COVID-19 measures advocated since the beginning of the pandemic.
Evidence has shown these measures to be effective in reducing COVID-19 cases and hospitalisation and in preventing deaths (WHO, 14 June 2021). Tracking of PHSM is being done by the WHO to collate data and provide a structure and taxonomy to these measures. Also included as PHSM are infection prevention and control measures such as contact tracing, surveillance, and genomic sequencing that aid in monitoring the SARS-CoV-2 trends and variants.
COVID-19 Vaccines in ASEAN
Vaccines are one of the most cost- effective and established global public health interventions used in the prevention of devastating infectious diseases. Access to safe and effective vaccines is a critical intervention that will help end the COVID-19 pandemic.
Through global and regional cooperation and solidarity in the COVID-19 response, enormous possibilities have been realised to support the availability and equitable distribution of COVID-19 vaccines globally. Such is the Gavi Advance Market Commitment for COVID-19 Vaccines (Gavi COVAX AMC), which is a mechanism that finances the procurement of COVID-19 vaccine doses for 92 low- and middle-income economies around the world (Berkley, n.d.). To support vaccine equity and to help ensure that no one is left behind, the WHO set out subsequent global targets to vaccinate at least 10 per cent of the population in every country by September 2021, at least 40 per cent by the end of 2021, and 70 per cent by the middle of 2022.
The Access to COVID-19 Tools (ACT)Accelerator was established to contain the COVID-19 pandemic faster and more efficiently by ensuring that successful diagnostics, vaccines and treatments are shared equitably across all countries (WHO, 9 September 2020). The vaccine pillar of the ACT-Accelerator is the COVAX facility that is co-led by CEPI, Gavi, and WHO, with UNICEF as the key delivery partner. COVAX aims to hasten the development and manufacturing of COVID-19 vaccines and ensure fair and equitable access for every country in the world.
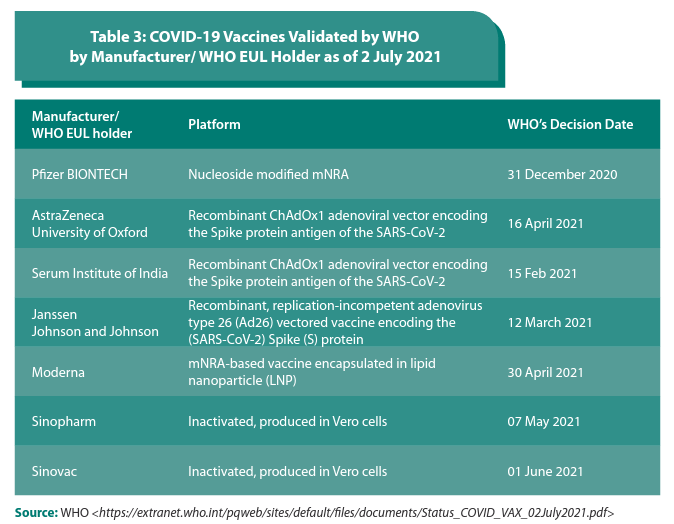
As of July 2021, there are 292 vaccine candidates with 108 vaccines under clinical development and 184 in pre-clinical development (WHO, 17 September 2021). A number of vaccine-producing ASEAN Member States, such as Indonesia, Thailand, Singapore, and Viet Nam have also endeavoured to contribute to COVID-19 vaccine development and manufacturing. To date, seven COVID-19 vaccines have received validation for emergency use from the WHO, and have been deployed in countries including ASEAN Member States (Table 2).
As part of the efforts to ensure adequate supplies and make vaccines available globally, 18.7 billion doses have been secured and more than 278 million doses have been shipped to 141 countries through COVAX, as of 15 September 2021. The price per vaccine dose ranges from 2 US dollars to 37 US dollars (UNICEF, 2021).
The vaccines that ASEAN Member States have procured through bilateral and multilateral arrangements, and have received through the COVAX contribute to their national vaccine campaigns and programmes. Based on the COVAX data, from March to June 2021, ASEAN Member States such as Cambodia, Indonesia, Lao PDR, Malaysia, the Philippines, and Singapore have received COVID-19 vaccines through the COVAX facility.
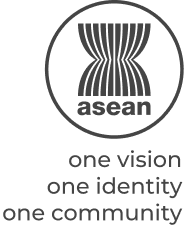
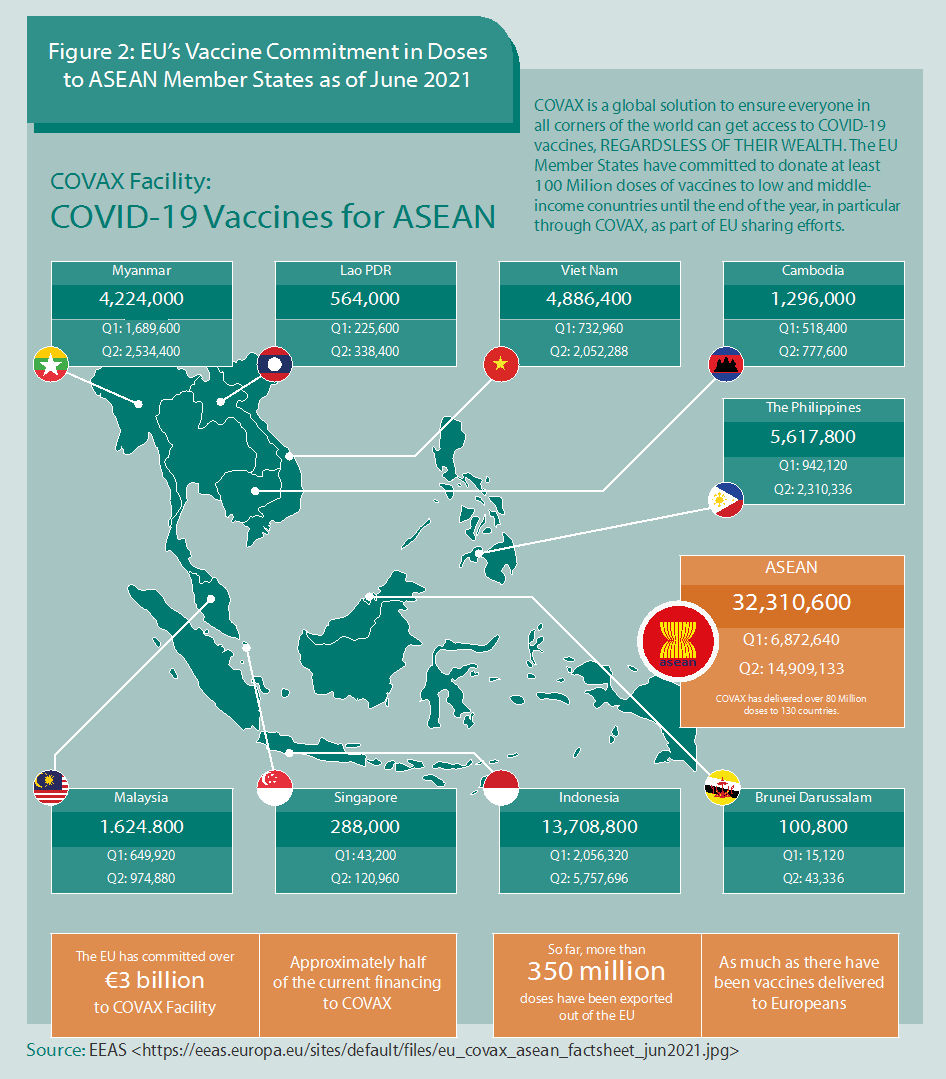
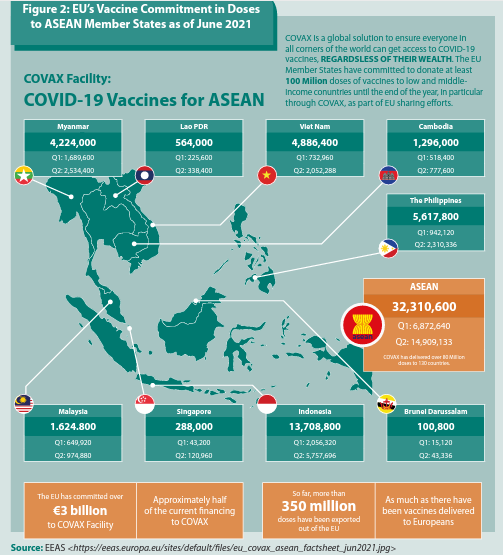
The European Union has coursed its substantial support to the ASEAN Member States through a multilateral route, including the COVAX mechanism. The EU and ASEAN have committed to fair, equitable, and affordable access to COVID-19 vaccines. Figure 2 below shows EU’s vaccine sharing efforts to ASEAN Member States amounting to more than 32 million doses.
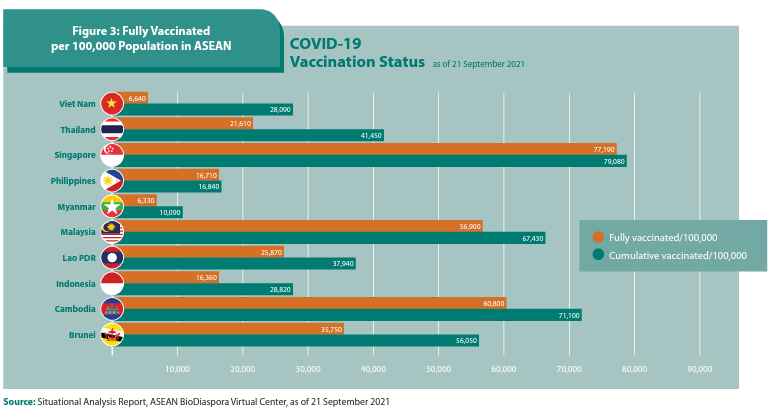
The progress of vaccinations in ASEAN Member States is monitored through the ASEAN Biodiaspora Virtual Centre. Based on its report, though the ASEAN Member States have been steadily progressing in terms of the vaccine coverage through their vaccine roll out programmes, a majority of the Member States have yet to reach their national and global targets (Figure 3).
Apart from limited access to safe and effective vaccines, other health system factors are affecting the rate of vaccination. These challenges include the availability of human resources for health to support the vaccination programme; providing cold chain maintenance and protection; sourcing transportation to reach remote areas; and, maintaining a steady supply of personal protective equipment and medical supplies necessary to support the vaccination programme.
To contribute to the global and AMS interventions, at the regional level, the ASEAN Leaders’ Declaration on ASEAN Vaccine Security and Self- Reliance (AVSSR) paved the way for the development, endorsement, and implementation of the Regional Strategic and Action Plan on AVSSR 2021-2025. It has five strategies which include the following:
i. Advance AVSSR into global policy level.
ii. Support the effective procurement strategies and establish the regional stockpiling mechanism.
iii. Establish or strengthen information sharing platforms to support AVSSR.
iv. Strengthen the capacity of the key stakeholders to achieve vaccine security in ASEAN.
v. Establish a monitoring and evaluation mechanism for the implementation of the plan, including communication and coordination mechanisms.

Vaccine Hesitancy, Infodemic, and COVID-19
Vaccine hesitancy is one of the challenges affecting current efforts to achieve the objectives of the national COVID-19 vaccine roll out programmes. It is one of the 10 threats to global health identified by WHO in 2019, and is defined as the “delay in acceptance or refusal of vaccines despite availability of vaccination services”. According to the WHO Sage Working Group on Vaccine Hesitancy, the lack of confidence, complacency, and the inconvenience of accessing vaccines are some of the common factors that underlie this complex concept.
Vaccine confidence refers to the effectiveness and safety of vaccines, the system that delivers them, including the reliability and competence of the health services and the health professionals and the motivations of the policy-makers who decide on the needed vaccines. Complacency happens when perceived risks of vaccine-preventable diseases are low, and vaccination is not deemed necessary as a preventive measure. Convenience refers to the physical availability, affordability and willingnessto-pay, geographical accessibility, ability to understand, quality of services and delivery in consideration of the cultural context and appeal of immunisation services affect uptake (WHO, 1 October 2014). Additional factors are calculation which pertains to an individual’s efforts to weigh costs and benefits, and collective responsibility pertains to the willingness to protect others from infection through one’s vaccination.
The COVID-19 pandemic is also aggravated and plagued by what is referred to as an information epidemic or “infodemic.” Apart from information on the SARS-COV-2 and its variants, there is also the prevalence of misinformation, disinformation, fake news, in traditional and social media platforms that churn out unverified and dubious information from non-credible sources. This infodemic undermines evidence-based information, contributes to vaccine hesitancy, and places people in vulnerable, even deadly situations.
Generally, approaches to address vaccine hesitancy are designed to be multi-pronged to increase knowledge, awareness, and vaccine uptake among the public. These approaches should counter misinformation and disinformation by building a communication ecosystem. Effective, appropriate, and sustained online and offline vaccination campaigns and communication strategies are a must to change people’s attitudes and behaviours, and to positively transform people’s perceptions to help them make informed decisions about COVID-19 vaccines.
n targeting key groups, such as unvaccinated or under-vaccinated populations and individuals or communities, there is a need to deliver transparent, consistent, frequent, appropriate, and positive messages through multiple communication platforms, including social media. Health workers, leaders in the health and non-health sectors, and other influential stakeholders should be empowered to deliver messages that are informed by data and science. Multiple strategies may be employed to counter vaccine hesitancy, and these include policy options such as mandatory vaccinations, sanctions for non- vaccination, different types of incentives, and vaccination reminders and follow-ups.
The development and emergency use of COVID-19 vaccines, within the first year of the pandemic, was unprecedented. Despite the emergence of new variants, the world can still be a step ahead of the virus if preventive health measures are in place, and if safe, effective vaccines are made available to everyone.
References:
ASEAN. (2021). ASEAN Health Sector Efforts in the Prevention, Detection, and Response to COVID-19. ASEAN website. Retrieved from https://asean.org/asean-health-sector-efforts-in-the-prevention-detectionand-response-to-coronavirus-disease-2019-covid-19-1/; Berkley, S. (n.d.). The Gavi COVAX AMC Explained. Gavi, The Vaccine Alliance website. Retrieved on 10 July 2021 from https://www.gavi.org/vaccineswork/ gavi-covax-amc-explained; UNICEF. (2021). COVID-19 Vaccine Market Dashboard. UNICEF website. Retrieved 15 September 2021 from https://www.unicef.org/supply/covid-19-vaccine-market-dashboard; WHO. (2014, October 1). Report of the Sage Working Group on Vaccine Hesitancy. WHO website. Rertieved from https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_ vaccine_hesitancy_final.pdf; WHO. (2021). COVID-19 Dashboard. WHO website. Retrieved 15 September 2021 from https://covid19.who.int/; WHO. (n.d.). Tracking SARS-COV-2 Variants. WHO website. Retrieved 2 July 2021 from https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/; WHO. (2021, March 1). The Effects of Virus Variants on COVID-19 Vaccines. WHO website. Retrieved from https://www.who.int/ news-room/feature-stories/detail/the-effects-of-virus-variants-on-covid-19-vaccines?gclid=EAIaIQobChMIjJmujouB8wIVCDErCh0IbgQ2EAAYASAAEgLH0PD_BwE; WHO. (2021, June 14). Considerations for Implementing and Adjusting Public Health and Social Measures in the Context of COVID-19. WHO website. Retrieved from https://www.who.int/publications/i/item/considerations-in-adjusting-public-health-andsocial-measures-in-the-context-of-covid-19-interim-guidance; WHO. (2020, September 9). Fair Allocation Mechanism for COVID-19 Vaccines through the COVAX Facility. WHO website. Retrieved 10 July 2021 from https://www.who.int/publications/m/item/fair-allocation-mechanism-for-covid-19-vaccines-through-the-covax-facility; WHO. (2021, September 14). Weekly Epidemiological Update on COVID-19–14 September 2021, Edition 57. WHO website. Retrieved from https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19—14-september-2021; WHO. (2021, September 17). COVID-19 Vaccine Tracker and Landscape. WHO website. Retrieved 27 Jul 2021 from https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines