






Introduction
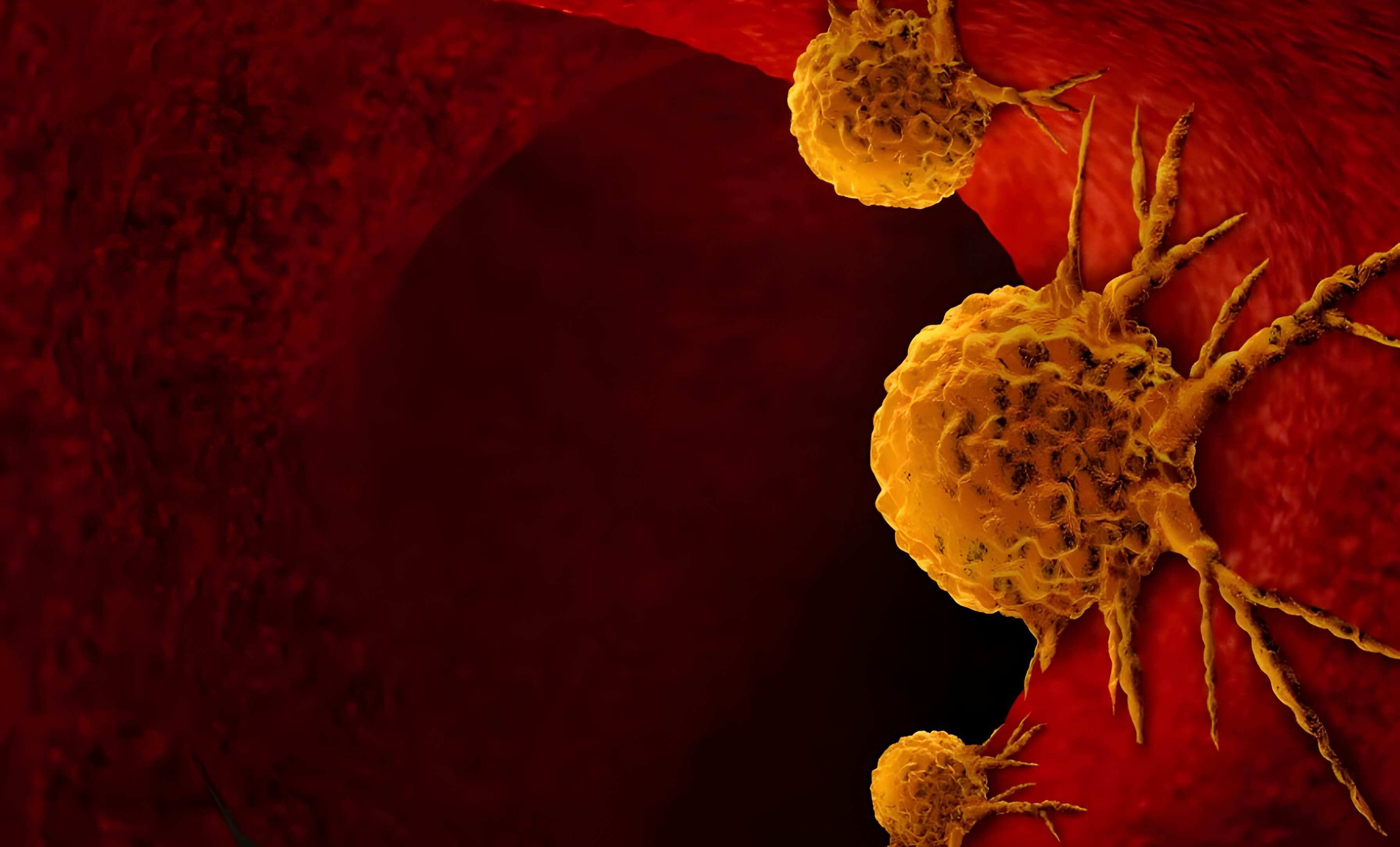
On 13 January 2020, the South-East Asia Region was thrust into an era of unprecedented turbulence with the confirmation of its first case of what was subsequently named COVID-19 in Thailand. Until the WHO revoked COVID-19’s health emergency status in May 2023, it had resulted in 61,275,290 infected patients and 808,604 deaths (ArcGIS, n.d.) in the WHO South-East Asia Region; globally, it had caused more than 765 million cases and nearly 6.9 million deaths (UN News, 2023). As the virus spread, countries faced a challenging journey of implementing public health measures amidst economic and social disruptions. Despite the challenges, they collaborated to strengthen healthcare capacity and pioneer solutions, navigating towards resilience for future crises.
Following the initial imported cases, the virus spread across countries through inter-and intra-country travel. Public and social health measures like travel restrictions, border closures, lockdowns, screening, quarantine, and social distancing measures were adopted, some ad hoc and more stringent than necessary. Although these measures aimed to slow transmission and prevent healthcare systems from becoming overwhelmed, they also caused economic distress and extreme, avoidable scenarios. For example, mass urban-to-rural like mass urban-to-rural migration in India, a surge in inter-border migration in Thailand, Bangladesh, etc., which strained points of entry. With the reliable support of international and private partners, governments expanded healthcare capacity by setting up dedicated COVID-19 treatment facilities, increasing hospital beds, and securing medical supplies and equipment, such as ventilators, personal protective equipment (PPE), testing kits, and medical oxygen.
However, hospitals faced shortages of medical supplies, equipment, and personnel, while non-COVID healthcare services were disrupted. Economically, lockdowns and restrictions led to disruptions in supply chains, affecting businesses and livelihoods. Socially, vulnerable populations faced heightened hardships, including job losses and food insecurity. Moreover, a lack of awareness perpetuated stigma towards COVID-19 patients and healthcare workers attending them, compounding the challenges faced by those already vulnerable and stretched.
What went well
Amidst the challenges posed by the COVID-19 pandemic, Member States in the region demonstrated remarkable resilience and innovation in their responses.
Diagnostics, laboratory capacity and genomic surveillance
Recognising the pivotal role of diagnostics in shaping and customising public health responses, the WHO, in collaboration with its partners, undertook comprehensive efforts to strengthen testing capacities across Southeast Asian countries (WHO, 2020a). Efforts to ensure widespread access to testing at sub- national levels included training laboratory staff, improving logistics, and enhancing data and quality management systems. Emphasising sustainability, these initiatives aimed to establish lasting infrastructure and systems that would continue to benefit communities beyond the immediate challenges posed by the pandemic (WHO South-East Asia Region, 2022).
Even though all countries were not evenly equipped to expand their capacities individually, regional and international cooperation helped mitigate the pandemic’s disastrous impact through proactive diagnostics, resource sharing, and collaborative response efforts.
Digital resources
Incorporating digital resources into the healthcare system during the pandemic emerged as a highly effective strategy. The widespread adoption and proficiency in using these platforms laid the groundwork for subsequent post-pandemic government health initiatives. In 2018, among the Member States, only Thailand had up-to-date official telemedicine guidelines. However, at the onset of the pandemic, India, Bangladesh, Indonesia, and Nepal published or updated their telemedicine guidelines (MarkWide Research, n.d.). As a result, online consultation has been institutionalised in various hospitals in these countries, and increasing trends in utilisation are being observed.
Utilising digital resources also played a crucial role in disseminating credible information and facilitating response efforts during the pandemic. All Member States spearheaded initiatives like COVID-19 Hotline Services and Health Information Portals. The widespread utilisation of these portals demonstrated the significance of digital tools in pandemic response. Intra-country app-based solutions like Myanmar’s Saw Saw Shar and India’s Arogya Setu enabled contact tracing. Sri Lanka’s SelfShield app provided real-time alerts, and platforms like CoWIN in India and Thai Chana in Thailand facilitated vaccination and symptom checking.
Leveraging established digital platforms as reliable sources of information bolstered public trust in and accessibility to official communication channels. It offered viable solutions for combating misinformation and disinformation, reducing stigma related to illnesses, fostering broader health awareness, and laying the foundation for addressing infodemics systematically.
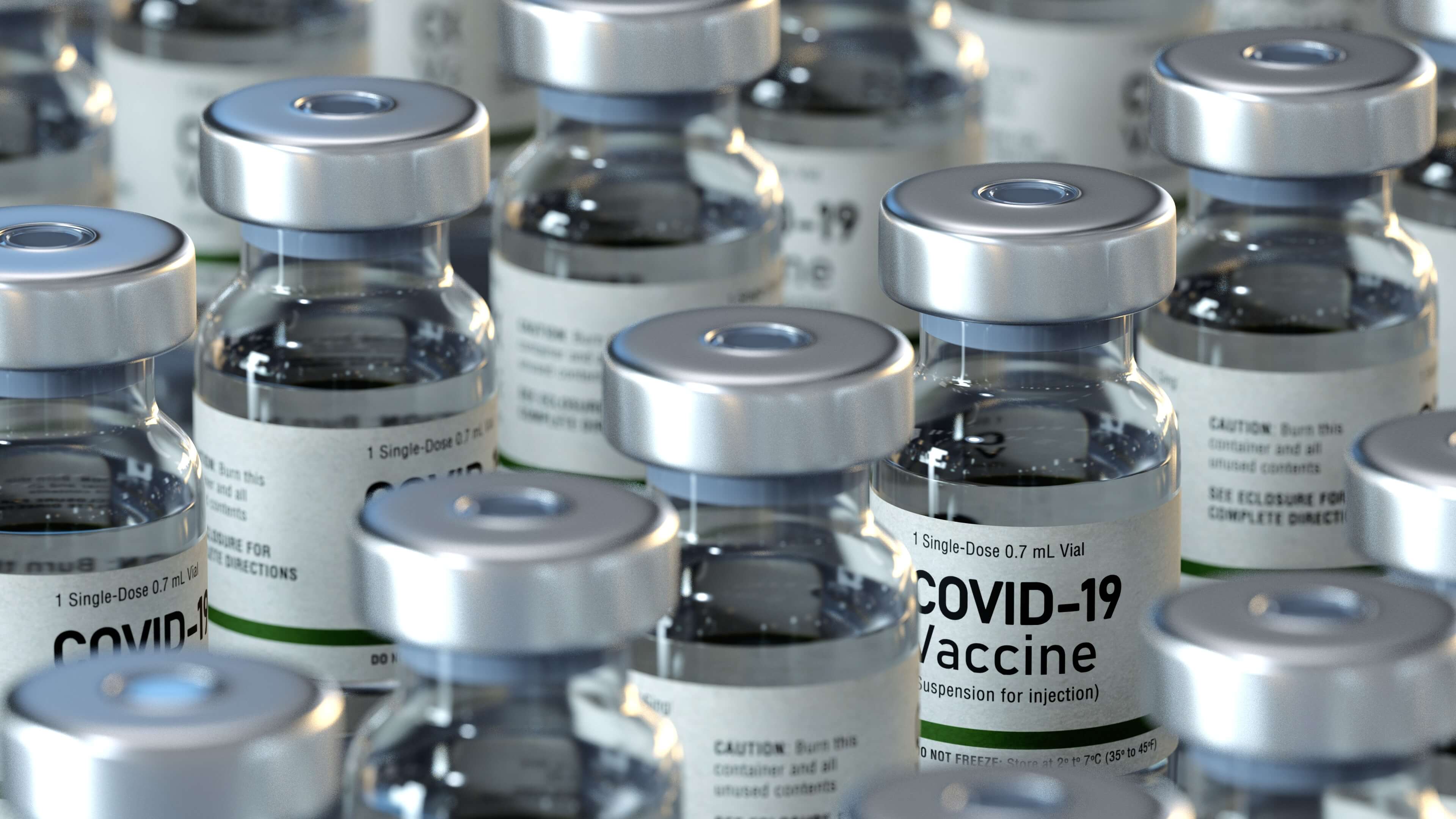
Vaccine production and deployment campaigns
Countries like India, Thailand (Economic Times Healthworld, 2021), and Indonesia (East Asia Forum, 2022) spearheaded vaccine production efforts, meeting a significant portion of domestic and global demands. India’s Vaccine Maitri initiative provided millions of doses to countries worldwide, while Indonesia’s Indovac garnered attention for its cost-effective model. Countries also invested in increasing production capacity, establishing sustainable long-term vaccine manufacturing, and promoting self-sufficiency (Biofarma, 2022). These efforts strengthened the region’s pharmaceutical sector and infrastructure, laying the groundwork for improved vaccine pipeline and preparedness for future health crises.
WHO also played a crucial role in developing and administering COVID-19 vaccines by facilitating regular meetings with national regulatory authorities, vaccine manufacturers (WHO South-East Asia Region, 2020), and international organisations such as GAVI and UNICEF (Tham, 2022).
Initially, vaccine hesitancy (WHO, 2015) emerged as a significant challenge to successfully implementing vaccination campaigns. WHO aided Member States in developing various approaches for addressing vaccine-related concerns and actively engaging with communities to build trust and confidence by rapidly addressing the “infodemic”. This was in collaboration with the regional partners such as UNICEF and the International Federation of Red Cross and Red Crescent Societies (IFRC).
Bhutan, Bangladesh, Nepal, and Thailand achieved more than 80 per cent coverage for the primary doses of vaccines. Other Member States achieved more than 60 per cent as a result of successful vaccination campaigns through extensive community engagement (WHO South-East Asia Region, n.d.).
What did not go well
Strain on critical care capacity
Despite efforts to expand capacity, accessing critical care remained challenging, particularly in remote and rural underserved regions. Hospitals became overwhelmed with COVID-19 patients, resulting in shortages of ICU beds, ventilators, oxygen supplies, and life-saving medications. Furthermore, the overwhelming focus on COVID-19 patients led to a compromise of other health concerns, including primary and preventive care, child vaccinations, mental health services, and the management of emergencies due to non-communicable diseases and maintenance of care.
Oxygen supply
The inadequate supply of oxygen and the collapse of its supply chain due to excess demand caused several preventable deaths in Bangladesh, Indonesia, Nepal, Sri Lanka, Thailand, Timor-Leste, and India. During the second wave in March 2021, more than half a million COVID-19 patients in lower-middle income countries were estimated to need oxygen treatment every day. Assessments showed that 90 million US dollars in immediate funding were required to meet urgent oxygen-related needs (Path, n.d.). Oxygen-producing facilities were often located far away from areas experiencing high demand, leading to logistical challenges in transporting oxygen to where it was needed most. Furthermore, the distribution of oxygen cylinders was poorly managed, with instances of price hikes and black-market activities reported. Despite efforts by governments, NGOs and other organisations to coordinate oxygen distribution, the shortages persisted.
Inequity
The COVID-19 pandemic highlights social disparities, impacting marginalised groups disproportionately due to factors like race, ethnicity, and socio-economic status. Studies showed vulnerable populations lacked adequate public health safeguards and faced many challenges. The world witnessed stigma towards positive cases, their families, and health workers who attended to them. Migrants, travellers, and refugees experienced discrimination. Stringent measures like closures worsened access to essential services and increased disparities and mental health risks. Vaccine distribution remains unequal, driven by profit and politicisation, furthering distrust and structural racism (WHO, n.d.; WHO, 2021a; Xiong & Peng L, 2020; Wouters, et al., 2021; Kelley et al., 2020).
Misinformation and rumours
Information overload and false information regarding the virus, treatments, and preventive measures circulated widely through public and private channels, inducing public uncertainty and panic. These inaccuracies led to misguided actions and hindered the efficacy of control measures implemented by governments. Scientific uncertainty that is part of an emerging issue and new disease was not optimally managed and communicated to the public by health authorities and experts.
Actions taken at the regional level post-pandemic
Build back better essential health services
In the post-COVID era, concerted efforts were made by both the Southeast Asia region and the WHO to enhance pandemic preparedness. These included the declaration on COVID-19 and measures to ”build back better”, improving essential health services, achieving universal health coverage and the health-related Sustainable Development Goals.
Regional roadmaps
Additionally, initiatives such as the South-East Asia Regional Roadmap for Diagnostic Preparedness, Integrated Laboratory Networking, and Genomic Surveillance (WHO, 2022a) and a Regional Strategic Roadmap on health security and health system resilience for emergencies spanning 2023–2027 were developed in consultation with Member States and partners by the WHO (WHO, 2022b). Both roadmaps were adopted by the SEAR Regional Committee of Health Ministers in 2022.
Good practices
Aided by the WHO Intra Action Review methodology and tools, countries diligently collected and shared their good practices, accumulating a wealth of valuable lessons learned (WHO, 2023). This knowledge-sharing endeavour aimed to facilitate better preparedness and prevention strategies for potential future pandemics. By leveraging the collective experiences and successes of diverse nations, the global community endeavours to strengthen resilience and response mechanisms, ultimately enhancing global health security and safeguarding against future infectious disease outbreaks.
What Next?
At the community level
There must be a concerted effort towards bolstering primary healthcare infrastructure and systems to lay the groundwork for Universal Health Coverage and integrative health systems. Programmes to increase health literacy and emergency preparedness need to be encouraged at the community level. Strengthening hygiene, sanitation, immunisation coverage, and food security can go a long way in preventing the spread of diseases and mitigating their impact. Decision-making processes must involve more local leaders, grassroots organisations, and community members as it leads to increased trust, which then ensures more effective implementation of policies and interventions that are co-created and owned by empowered communities.
At the country level
As the world transitions from the acute phase of the COVID-19 pandemic, it is imperative to refocus attention on the multitude of health concerns that were sidelined during the crisis. A crucial step forward involves repurposing the infrastructure developed for the pandemic response to address these neglected areas. For instance, the vaccine distribution network addressing a range of age groups not usually covered by previous routine immunisation mechanisms can be seamlessly integrated into immunisation programmes to ensure broader coverage and accessibility.
While the pandemic prompted a surge in health investments, ensuring continuous, institutionalised, and systematic allocation of resources remains imperative. This entails a paradigm shift in budgetary allocations towards health sectors, especially for preparedness and health system resilience, and not merely for health care, as evidenced by the static and fluctuating trends observed in the South-East Asia Region countries during and after the pandemic.
At the regional level
Robust knowledge-sharing mechanisms must be established to disseminate best practices and facilitate intersectoral and cross-country learning (WHO, 2021b). By investing in preventive measures and promoting general wellness, countries can effectively mitigate the risk of future pandemics and enhance overall population health. Prioritising and safeguarding vulnerable populations across the region should be central tenets of these revamped policies underpinned by a commitment to sustainable health practices. Further, sustainable pandemic preparedness funding is paramount for long-term resilience, necessitating steady investment in health infrastructure.
To ensure regional health security, Member States should consider establishing a robust regional-level health security governance mechanism, such as the Regional Health Emergency Council. This council would enable active engagement from the highest levels of government, including state functionaries, fostering solidarity and effective inter-country cooperation and collaboration.
By adopting a comprehensive approach that integrates pandemic infrastructure, strengthens primary healthcare systems, and fosters sustainable funding mechanisms, we can collectively pave the way for resilient national health systems. These robust systems, buttressed by the required regional mechanisms that catalyse and support national institutes, will be capable of weathering future challenges.
Note:
The WHO South-East Asia Region Member States include Indonesia, Myanmar and Thailand.
The views and opinions expressed in this article are solely those of the author and do not reflect the official policy or position of ASEAN.